Angioplasty and Stenting in Peripheral Vascular Conditions
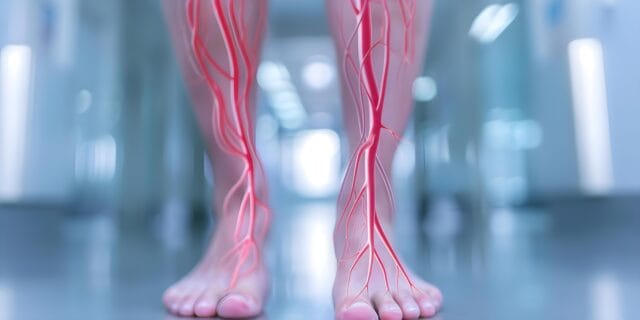
Angioplasty and stenting in peripheral vascular territories constitute a foundational approach in the contemporary management of peripheral artery disease (PAD) and a range of extra-coronary vascular disorders. These endovascular procedures aim to re-establish adequate perfusion in arterial segments compromised by luminal narrowing or occlusion, thereby preserving tissue viability and preventing ischemic complications. While coronary interventions focus exclusively on the myocardial circulation, peripheral angioplasty and stenting are applied to extracardiac arterial systems, including—but not limited to—the lower extremity vasculature, renal arteries, mesenteric vessels, and carotid arteries. These vascular beds are critical for maintaining the function of organs and tissues outside the heart, and impairment in their blood supply can lead to significant morbidity and mortality if not promptly addressed.
Depending on clinical urgency, these procedures may be performed electively for progressive but stable ischemia or emergently in limb- or organ-threatening situations. Their execution is typically performed by vascular surgeons, interventional radiologists, or other specialists with expertise in catheter-based techniques. As a result, angioplasty and stenting in peripheral territories have evolved into common practices for limb salvage, cerebral perfusion preservation, and renal or visceral organ protection.
FOR PATIENTS REQUIRING EMERGENCY TREATMENT, IT IS ESSENTIAL TO SEEK IMMEDIATE MEDICAL ATTENTION AT THE NEAREST EMERGENCY FACILITY FOR URGENT CARE.
Why Cuba:
Elective endovascular intervention for peripheral vascular conditions in Cuba is delivered with a strong emphasis on restoring blood flow, preserving limb function, and preventing life-altering consequences such as amputation, stroke, or organ failure. The approach to angioplasty and stenting is highly individualized, taking into account the location of arterial compromise, the severity of the obstruction, and the patient’s broader medical condition to ensure both safety and effectiveness.
Cuban specialists utilize advanced imaging and diagnostic technologies to precisely identify vascular abnormalities and formulate intervention strategies. When suitable, minimally invasive procedures such as balloon angioplasty and stent placement are prioritized, offering patients reduced procedural trauma, faster recovery times, and minimal disruption to surrounding structures. For complex or advanced cases requiring surgical access, interventions are performed by skilled teams trained in both open and hybrid techniques.
Care does not end in the operating suite. A multidisciplinary framework ensures that patients receive comprehensive follow-up, including rehabilitation planning, vascular health monitoring, and lifestyle guidance aimed at preventing recurrence and supporting long-term vascular integrity. This integrative model reflects Cuba’s broader commitment to accessible, outcomes-focused vascular care grounded in clinical precision and compassion.
Conditions Treated by Elective Peripheral Angioplasty and Stenting
Elective angioplasty and stenting are commonly performed to treat chronic, non-urgent cases of:
- Peripheral Artery Disease (PAD) in the lower extremities, resulting in claudication or mobility limitations.
- Renal Artery Stenosis, which may contribute to hypertension or mild renal insufficiency.
- Carotid Artery Stenosis, identified prior to the onset of stroke symptoms.
- Mesenteric Artery Stenosis, causing chronic mesenteric ischemia, such as postprandial abdominal pain and weight loss.
The most prevalent underlying cause of these conditions is atherosclerosis—a degenerative vascular condition characterized by the accumulation of cholesterol-rich plaque within arterial walls. Over time, these plaques reduce arterial lumen diameter, limiting oxygen-rich blood flow to distal tissues. Risk factors contributing to atherosclerosis include:
- Smoking
- Diabetes mellitus
- Hypertension
- High cholesterol
- Sedentary lifestyle
- Family history of cardiovascular disease
These risk factors collectively contribute to progressive vascular narrowing, eventually warranting interventional correction when symptoms emerge, or perfusion is compromised.
Indications for Elective Angioplasty and Stenting in Peripheral Artery Disease
Elective angioplasty and stenting are typically recommended when conservative medical management—including medications and lifestyle modifications—fails to alleviate symptoms or halt disease progression. These procedures are not performed in emergencies but rather scheduled based on diagnostic findings and clinical indicators such as:
- Lifestyle-limiting leg pain (claudication)
- Documented arterial stenosis exceeding 50–70%
- Early signs of end-organ dysfunction (e.g., reduced renal perfusion or cerebral flow)
Failure to address chronic vascular narrowing in a timely manner can lead to:
- Worsening symptoms and reduced mobility
- Transition from elective to emergency status (e.g., development of critical limb ischemia)
- Risk of irreversible tissue or organ damage
- Increased likelihood of requiring open surgical intervention or amputation
Timely elective procedures help preserve function, enhance quality of life, and reduce long-term health risks.
Qualification for Elective Peripheral Angioplasty and Stenting
Candidates for elective peripheral angioplasty and stenting typically include patients with:
- Diagnosed moderate to severe arterial stenosis with associated symptoms
- Poor response to medical therapy or lifestyle changes
- Favorable vascular anatomy suitable for catheter-based intervention
- Acceptable perioperative risk profile, as determined by clinical evaluation
Eligibility is assessed using a combination of clinical history, symptom assessment, vascular imaging, and overall health status to ensure optimal outcomes and safety.
Pre-Surgery Diagnosis
Prior to elective angioplasty and stenting, patients undergo thorough diagnostic assessment to confirm the presence, location, and severity of arterial disease. This includes:
- Ankle-Brachial Index (ABI) to evaluate limb perfusion
- Duplex Ultrasonography to visualize blood flow and stenosis
- CT Angiography or MR Angiography for detailed anatomical mapping
- Digital Subtraction Angiography (DSA) as a definitive intraoperative tool
Comprehensive cardiovascular risk profiling is also conducted to assess candidacy and guide perioperative management.
Types of Angioplasty and Stenting
A variety of endovascular strategies may be employed in elective peripheral angioplasty and stenting, with the specific technique tailored to the patient’s vascular anatomy, the characteristics of the lesion, and the long-term therapeutic goals. These techniques are designed to restore and sustain arterial blood flow while minimizing trauma to the vessel wall and surrounding tissues.
Balloon Angioplasty (Percutaneous Transluminal Angioplasty – PTA)
- Involves the use of a catheter with an inflatable balloon at its tip.
- The catheter is guided to the site of arterial stenosis.
- The balloon is inflated under high pressure to:
- Compress atherosclerotic plaque against the arterial wall.
- Widen the vessel lumen, improving blood flow.
- Often used as the initial step in endovascular revascularization.
- May be performed:
- As a standalone procedure, or
- In conjunction with stent placement to maintain long-term patency.
- Stenting is typically considered if there is significant risk of vessel recoil or restenosis.
Bare-Metal and Drug-Eluting Stents (DES)
- Stents are commonly placed after balloon angioplasty to scaffold the artery and maintain vessel patency.
- Bare-metal stents (BMS):
- Provide mechanical support to the arterial wall.
- Help prevent vessel recoil and immediate restenosis.
- Drug-eluting stents (DES):
- Coated with pharmacological agents (e.g., sirolimus, paclitaxel).
- These drugs inhibit neointimal hyperplasia, a key factor in restenosis.
- DES are especially beneficial in:
- Small-diameter arteries.
- Lesions with a high risk of re-narrowing after angioplasty.
Covered Stents (Stent Grafts)
- Also known as stent grafts.
- Consist of a metallic stent framework covered with a synthetic outer layer (e.g., expanded polytetrafluoroethylene or Dacron).
- The synthetic covering acts as a barrier to blood flow through damaged vessel walls.
- Commonly used in cases involving:
- Arterial dissection.
- Aneurysmal segments.
- Lesions with a high risk of rupture.
- Also effective in:
- Sealing arterial perforations.
- Excluding thrombus-containing segments from the bloodstream.
The selection among these endovascular modalities is influenced by a combination of anatomical factors (such as vessel diameter, location, and length of the lesion), clinical considerations (such as patient comorbidities and risk of restenosis), and operator experience. Each approach is intended to optimize arterial patency, restore perfusion, and reduce the need for more invasive surgical procedures, thereby enhancing both short-term recovery and long-term outcomes in patients undergoing elective treatment for peripheral vascular disease.
Minimally Invasive Procedure
Elective angioplasty and stenting for peripheral arteries are almost exclusively performed using minimally invasive (endovascular) techniques. Access is typically gained through a small puncture in the femoral, radial, or brachial artery, using image-guided catheter navigation to reach the affected site.
Benefits of Minimally Invasive Approaches
- Reduced hospital stay
- Less post-operative discomfort
- Faster return to daily activities
- Lower risk of infection and scarring
- No need for general anesthesia in most cases
Open surgical bypass may be considered if endovascular methods are not viable due to complete arterial occlusion, diffuse disease, or failed prior interventions.
